The HPA Axis
After the adrenals release epinephrine and all parts of the body have been given access to all potential sources of energy, the second aspect of the stress response system activates. This next step in the response involves what is known as the HPA axis.
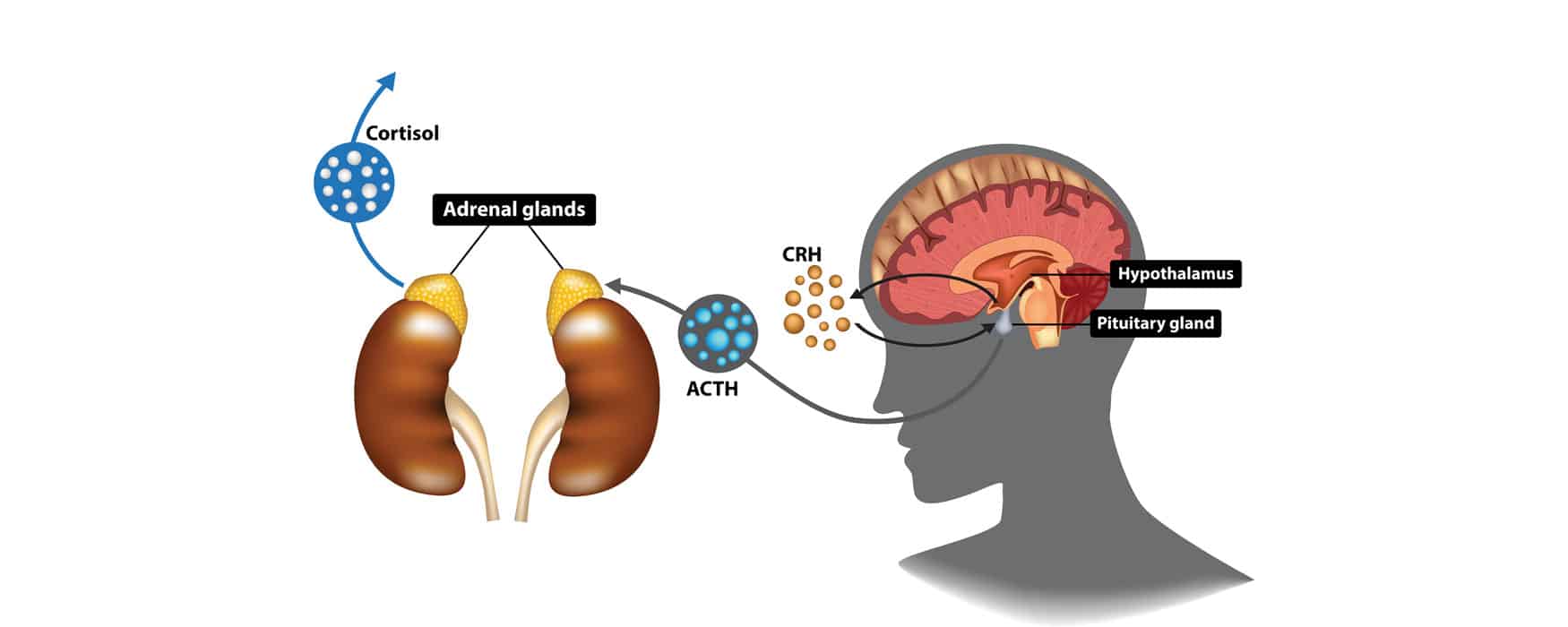
HPA is an acronym for hypothalamus, pituitary, and adrenals. The HPA axis is responsible for keeping the stress response going. It acts to sustain the stress response in the body through sets of hormonal signals.
First, the hypothalamus sends corticotropin-releasing hormone (CRH) to the pituitary gland. The pituitary gland is then triggered to release adrenocorticotropic hormone (ACTH), which travels to the adrenals. This signal, in turn, triggers the release of cortisol. Through the release of these hormones, the body stays on high alert status.
When the potential threat is removed, these elevated hormonal levels return to normal status, and the stress response is released. The sympathetic nervous system is then disengaged, and the body returns to homeostasis, a state of balance—that is, under “normal” circumstances.
However, with chronic stress, potential perceived threats are more frequent and can sometimes cause the body to stay on high alert for prolonged periods, thus causing the body to sustain unusually high levels of these hormones for too long—so often and so long that there are serious and lasting health implications.
Within the autonomic nervous system, we have both the sympathetic and parasympathetic nervous systems guiding the body’s physiological responses. The sympathetic, again, puts us on alert for potential dangers and gives us the “juice” to fight or flee.
In the converse, the parasympathetic nervous system tells us it’s okay to relax. It is activated when we feel safe, when we are in a safe location, when we perceive no potentially dangerous threats around us.
When the parasympathetic nervous system is activated, we feel calm. Our bodies reflect this through
- Lower blood pressure
- Lower heart rate
- Slower pulse
- Even breathing
- Lower cortisol levels
- Lower adrenaline (epinephrine).
Our bodies are allowed then to “rest and digest” rather than being on our guard—two things the stress response prevents our bodies from doing properly.